I have been writing about our experiences with eczema (or more specifically Atopic Dermatitis) for almost 2 years now. I have written about the various treatments we have tried in various posts but I realised that I have not really written in details and in a comprehensive manner about the first, second line and third line treatments that are usually used to treat eczema.
(Please note: I will refer to Atopic Dermatitis as eczema in my post from here on to simplify matters)
In this post I have written about the regular medical treatment that is used once the moisturisers alone are not able to control the inflammation. Moisturisers are an essential part of the treatment for eczema and works very well in mild forms but may not be sufficient to bring the eczema under control once the skin becomes red and inflamed in moderate to severe eczema. I have myself been confused at times with the myriad topical, steroidal and non steroidal creams that are prescribed by the doctors at various points in time. Then there are also the oral steroid medications and different immunosuppressants and phototherapy treatment that we have used to control flare ups. I believe it would help a lot of parents (and those adults suffering from eczema) if they had some idea about the basics of the different types of treatments and medications that they may be using on their child or even on themselves. It would definitely help in controlling and reducing the side effects that some of these strong medications can have on a person if not used properly.
Topical steroids

Topical corticosteroids are prescribed by the doctor/dermatologist when the skin becomes red and inflamed and the eczema does not clear up in spite of maintaining a healthy and regular bathing and moisturising routine. The topical corticosteroids range from very mild to very potent and you should be very careful in following the doctor’s instructions in using the same for your child both in terms of quantity and duration. This is especially true for young children and babies. In any case, the topical corticosteroids are prescribed only when the risks from eczema far outweigh the risks from the side effects of using these medicines. When a child suffering from eczema is unable to sleep at night due to incessant itching and thus starts affecting daily life at school and home, there is a risk of infection due to the cuts and inflamed skin, it is wise to use steroid creams/ointments as per the doctor’s advice till the time the rashes have gone.
Some important points to remember while using these medications-
- One should start using the lowest potency steroid and only step up if required
- Topical steroids are most effective if applied immediately after a bath but should only be applied on affected areas and not as a moisturiser
- One should follow the doctor’s advice on the frequency of application (usually twice a day is more than enough on severely inflamed skin) and should start tapering off as instructed instead of stopping abruptly
- Step up and the step down method (in terms of potency and frequency of steroid) needs to be maintained while using the topical steroids to keep the risks of side effects of these medications as low as possible
- One should avoid using these medications on the face and other sensitive areas and this is all the more true for children who have very sensitive and delicate skin
Given below are the various common (but certainly not exhaustive) topical corticosteroid creams/ointments that are available in India (and ones I am most familiar with) and their potency
- Low potency– Hydrocortisone creams (1%) are available as an OTC (over the counter) medicine in various forms like cream, ointment and lotions. This is the least potent amongst all the topical steroids but still should be used with caution especially for a child. This is especially true since this is easily available and one can unknowingly use this as a moisturiser without realising that it is still a steroid cream/ointment
- Mild to mid potency– Steroidal creams/ointments like Desonide, Mometasone fuorate and Fluticasone propionate are available at the lower to mid end of the potency spectrum. These are brands like Desowen, Momate/Elocon and Flutivate brands in India for the respective steroidal creams/ointments respectively. The doctors will prescribe a particular steroidal cream based on the level of inflammation and rashes
- Potent to highly potent– Steroidal creams like Betamethasone dipropionate and Halobetasol propionate are at the potent end of the corticosteroidal creams/ointment. In India we have brands like Fucibet (which also includes fucidic acid which is an antibacterial medication) and Halovate which include these steroids respectively.
You should also know there is an overlap in these topical medications since they are usually available in both cream and ointment forms and the potency for the same dosage will differ based on the form. The cream form has roughly half water and half oil, they spread easily, are well absorbed and usually wash off with water. Ointments on the other had are about 80% oil and 20% water and are thus “occlusive” which means they trap moisture and help in better absorption of the main component. Being occlusive, an ointment will allow the medication to get absorbed much more completely than a cream and hence are more potent at the same dosage as a cream.
https://www.psoriasis.org/sublearn03_mild_potency
Application and side effects
Topical corticosteroids should be used in a step up manner in terms of increasing potency starting from a low potency and only moving up if required. Usually the doctor will prescribe the milder ones like desonide cream (brand name- Desowen) and only graduate to a stronger medication like Fucibet if required later on. Similarly, once the rashes have been brought under control, one should use the step down method both in terms of potency as well as frequency as per the doctor’s instructions.
As mentioned earlier, these medications should only be applied on affected areas and not as a moisturiser. However, sometimes the rashes may be quite widespread all over the body. In that case, the doctor may prescribe a 1:4 ratio of a mild potency steroid like desowen to an emollient like cetraban which is then mixed thoroughly and applied all over the affected areas.
Side effects from these steroidal creams are varied and depends on the age of the person, the frequency of application, the potency of the drug amongst other factors. The thinning of the skin or skin atrophy is one such side effect which can take place if potent to highly potent steroidal creams are applied too frequently or without any break. However, one can avoid this and other side effects by following the doctor’s instructions for using this treatment and thus using this treatment as and when required, in the required quantity and for an appropriate duration. The other thing to keep in mind that in case of excessive scratching due constant itchiness in case of under medication, the skin tends to become thick and discoloured. Thus the treatment needs to be carried out in a timely manner under the supervision of a doctor and the instructions should be properly followed to minimise the side effects.
(Further reading-http://www.eczema.org/corticosteroids)
Calcineurin inhibitors
Another type of topical treatment available for eczema is the group of medications known as Calcineurin inhibitors. These are non-steroidal immunomodulators and are of 2 types- pimecrolimus 1% (Pacroma and Elidel) and tacrolimus 0.3% (Protopic). These topical medications work by suppressing the immune system and are usually prescribed to children over 2 years of age and adults and are recommended for use as a second line treatment for eczema.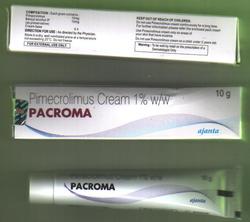
 As with steroidal medications, these type of immunomodulators should also be applied only when prescribed by the doctor and for the recommended duration of time. Even though it does not have the side effects like thinning of the skin which is associated with steroidal treatments, one still has to be cautious while using these medications since they are relatively new medications and not much is known about their long term usage. There is a possible risk of skin cancer only in the long run after prolonged usage but it is still advisable to apply these creams at night to avoid sunlight exposure. These medications are also prescribed for eczema on the face (unlike topical steroids) and are prescribed for moderate to severe eczema only when the combination of topical steroids and emollients have not been successful.
As with steroidal medications, these type of immunomodulators should also be applied only when prescribed by the doctor and for the recommended duration of time. Even though it does not have the side effects like thinning of the skin which is associated with steroidal treatments, one still has to be cautious while using these medications since they are relatively new medications and not much is known about their long term usage. There is a possible risk of skin cancer only in the long run after prolonged usage but it is still advisable to apply these creams at night to avoid sunlight exposure. These medications are also prescribed for eczema on the face (unlike topical steroids) and are prescribed for moderate to severe eczema only when the combination of topical steroids and emollients have not been successful.
(Further reading- http://www.ncbi.nlm.nih.gov/books/NBK45568/
http://www.ncbi.nlm.nih.gov/pubmed/14693489)
Phototherapy or Narrow band UVB

Another treatment that is prescribed once the topical treatments have not really worked for a person in controlling the eczema is phototherapy. It is used as a safer alternative to avoid using the third line treatments of the powerful immunosuppressive medications like azathioprine, methotrexate and cyclosporine.
In this treatment light or a particular narrow band of Ultraviolet rays are used to treat the eczema which is beneficial for skin diseases. It can be used both for localised as well as general areas of the skin covering the entire body. This treatment works effectively for some people but not for everyone and usually takes about 1 to 2 months to show the desire results. If this treatment is effective then it can effectively put the eczema in remission for a while at least. It may also minimise the usage of topical steroids and there its side effects.
Phototherapy is carried out in a special booth filled with UV rays for general treatment of eczema all over the body and hand-held devices for treatment of specific areas like hands, ankles etc. Nowadays, a high intensity phototherapy treatment is available in the form of a laser called Excimer. It is much more powerful than the regular phototherapy and emits Ultraviolet rays of a particular frequency which is used to treat different skin conditions like eczema, psoriasis etc. It is given in the form of a hand-held gadget and takes much less time than a regular phototherapy due to the high intensity of the rays and is more useful for treatment for localised areas of the body. However, one needs to be careful in protecting the eyes when undergoing this treatment. The risks associated with prolonged treatment are skin burns, increased ageing and increased risk of skin cancer. Like any other such treatment this has to be carried out under the supervision of a medical professional and all the instructions need to be followed carefully. (I have written about our experience with phototherapy in my blog post https://eczema-anindianperspective.com/2013/10/17/when-the-going-gets-tough-part-1/).
(This treatment is currently offered in the Comprehensive Skin Care Clinic run by senior pediatric dermatologist Dr Manish Shah in South Mumbai and the website is http://www.cscc.co.in/)
Oral Steroids

The third line of treatment for eczema is the use of systemic medications like oral steroids. Prednisone is one of the most commonly used oral steroids given in cases of severe eczema where an immediate result is required and is given under strict supervision of the doctor. It is given as a daily dose starting with a high dosage and then is slowly tapered down once the eczema is under control. Oral steroids work by suppressing the immune system and helps in controlling the overactive immune system in the case of a person suffering from eczema. But this also makes it possible for the person to catch infections easily due to a weakened immune system and hence has to be monitored at all times. Also, in the case of a child, oral steroids may slow down growth and development and hence again one needs to be very careful.
There are other side effects as well which can be minimised by following instructions carefully and keeping a lookout for any symptoms which may arise on taking this medication. This is also done by carrying regular blood tests to determine adverse side effects if any. Due to the various side effects of this medication and its quick action, oral steroids are usually prescribed for short periods of time when results are needed fast. Bottomline, like any strong medications, one needs to take this under strict supervision and follow the doctor’s instructions about dosages and how to start and stop taking this medication.
(Further reading: http://www.ncbi.nlm.nih.gov/books/NBK260241/)
Immunosuppressive medications

The other third line of systemic treatments include the immunosuppressive medications like azathioprine, cyclosporine and methotrexate. These are all very powerful medications and are given only when all other options have failed to yield the desired results. All of these medications work by suppressing the immune system and hence bring the eczema under control. But once again, due to the various side effects these medications have to be given under strict supervision of the doctor prescribing this and by following all the instructions carefully. Since eczema is a chronic condition and these medications may be required to be given for long periods of time, regular testing is required to ensure that there are no side effects.
Azathioprine
Azathioprine works by tweaking the growth of certain white blood cells which contribute to the inflammation associated with eczema and thus suppresses the immune system. It takes a while longer to show results than cyclosporine and may not suitable for acute flare ups.The main side effect of azathioprine is bone marrow suppression and that is why a specific test is carried out before prescribing this medication which is called the TPMT enzyme test. This test determines the suitability of the person by determining the ease by which the person is able to break down azathioprine in the normal way. However regular testing would be required to keep a track of any adverse effect on the immune system. This medication is taken orally in the form of tablets and on a daily basis in the prescribed dosage.
We had a traumatic experience with this medication which was prescribed by a leading pediatric dermatologist in London for our then 7 year old daughter. In her case, even though she had a normal TPMT result, her body reacted disastrously to this medication and she suffered from bone marrow suppression and had to fight for her life. This was a one in a million kind of event and has never happened before to someone with normal TPMT levels. I have written about our experience in my post in 2013 and you can read about it at https://eczema-anindianperspective.com/2013/10/27/the-tough-get-going-part-2/.
Cyclosporine
Cyclosporine is another systemic immunosuppressant used to bring severe eczema under control and works by specifically blocking an important pathway in the immune system, and has different side effects than steroids. It is prescribed in low doses for eczema under strict supervision and once the eczema is under control, the medication is tapered off. One of the main risks associated with this medication is damage to the kidney especially with increased dosage and duration of medication and hence regular tests would be required to monitor the kidney activity. This medication has to be taken orally on a daily basis as per the prescribed dosage.
(I have written more about our experience of dealing with cyclosporine and azathioprine medications in my blog post where I have compared both at https://eczema-anindianperspective.com/2014/02/10/azathioprine-and-cyclopsorin-an-overview-of-two-immunosuppressive-medicines-used-to-control-my-daughters-eczema-from-a-parents-point-of-view/).
Methotrexate
Methotrexate is another systemic immunosuppressant which is used mainly in treatment for psoriasis and different types of arthritis. It is also given in low doses in cases of severe eczema and usually takes longer to work than cyclosporine. It has anti inflammatory properties and works by altering the body’s use of folic acid (a vitamin) which is needed for cell growth. Thus a folic acid supplement is a must on a daily basis for those taking this medication. This medication is taken once a week in the form of tablets. This dosage may also be split up into 2 doses taken within 24 hours to minimise any nausea that may occur. One of the main possible side effects of this medication is again adverse effects on the immune system especially on the white blood cells (which fight infection) and platelets (which help stop bleeding). Thus regular blood tests are required to keep a look out for any adverse side effects.
(Further reading- http://rheuminfo.com/medications/methotrexate/methotrexate-detailed-information)
Sometimes the hardest thing and the right thing are the same

Sometimes we don’t have a choice as far as giving strong medications to our child is concerned when the child is suffering from a severe chronic condition which adversely affects daily living. Of course we would prefer to find some alternative which is much safer and without any of the side effects that I have mentioned above. As of now we have not managed to bring our daughter’s eczema into remission and she needs constant medication in order to live a relatively normal life.
Things can also go horribly wrong like it did in our case in spite the very best of intentions. We have been very lucky and have learned to take this in our stride and be more vigilant in the future since our daughter still requires immunosuppressants to keep her severe eczema under control. This has not stopped us from looking for other options and neither should you. As one wise person had said, it does not matter how slowly you go as long as you do not stop.